Identifying the most effective cancer treatment for a given patient from the get-go can help improve outcomes. Leslie Lauren/iStock via Getty Images Plus
Despite many efforts to find better, more effective ways to treat cancer, it remains a leading cause of death by disease among children in the U.S.
Cancer patients are also getting younger. Cancer diagnoses among those under 50 has risen by about 80% worldwide over the past 30 years. As of 2023, cancer is the second-leading cause of death both in the U.S. and around the world. While death rates from cancer have decreased over the past few decades, about 1 in 3 patients in the U.S. and 1 in 2 patients worldwide still die from cancer.
Despite advances in standard cancer treatments, many cancer patients still face uncertain outcomes when these treatments prove ineffective. Depending on the stage and location of the cancer and the patient’s medical history, most cancer types are treated with a mix of radiation, surgery and drugs. But if those standard treatments fail, patients and doctors enter a trial-and-error maze where effective treatments become difficult to predict because of limited information on the patient’s cancer.
My mission as a cancer researcher is to build a personalized guide of the most effective drugs for every cancer patient. My team and I do this by testing different medications on a patient’s own cancer cells before administering treatment, tailoring therapies that are most likely to selectively kill tumors while minimizing toxic effects.
In our newly published results of the first clinical trial combining drug sensitivity testing with DNA testing to identify effective treatments in children with cancer, an approach called functional precision medicine, we found this approach can help match patients with more FDA-approved treatment options and significantly improve outcomes.
What is functional precision medicine?
Even though two people with the same cancer might get the same medicine, they can have very different outcomes. Because each patient’s tumor is unique, it can be challenging to know which treatment works best.
To solve this problem, doctors analyze DNA mutations in the patient’s tumor, blood or saliva to match cancer medicines to patients. This approach is called precision medicine. However, the relationship between cancer DNA and how effective medicines will be against them is very complex. Matching medications to patients based on a single mutation overlooks other genetic and nongenetic mechanisms that influence how cells respond to drugs.
Functional precision medicine involves testing drugs on tumor samples to see which ones work best.
How to best match medicines to patients through DNA is still a major challenge. Overall, only 10% of cancer patients experience a clinical benefit from treatments matched to tumor DNA mutations.
Functional precision medicine takes a different approach to personalizing treatments. My team and I take a sample of a patient’s cancer cells from a biopsy, grow the cells in the lab and expose them to over 100 drugs approved by the Food and Drug Administration. In this process, called drug sensitivity testing, we look for the medications that kill the cancer cells.
New clinical trial results
Providing functional precision medicine to cancer patients in real life is very challenging. Off-label use of drugs and financial restrictions are key barriers. The health of cancer patients can also deteriorate rapidly, and physicians may be hesitant to try new methods.
But this is starting to change. Two teams in Europe recently showed that functional precision medicine could match effective treatments to about 55% of adult patients with blood cancers such as leukemia and lymphoma that did not respond to standard treatments.
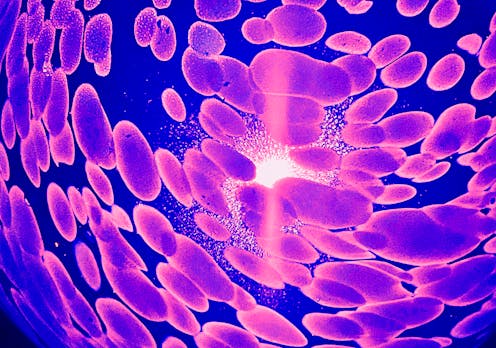
Most recently, my team’s clinical trial focused on childhood cancer patients whose cancer came back or didn’t respond to treatment. We applied our functional precision medicine approach to 25 patients with different types of cancer.
Researchers are testing a functional precision medicine approach to cancer treatment in both children and adults.
Pornpak Khunatorn/iStock via Getty Images Plus
Our trial showed that we could provide treatment options for almost all patients in less than two weeks. My colleague Arlet Maria Acanda de la Rocha was instrumental in helping return drug sensitivity data to patients as fast as possible. We were able to provide test results within 10 days of receiving a sample, compared with the roughly 30 days that standard genomic testing results that focus on identifying specific cancer mutations typically take to process.
Most importantly, our study showed that 83% of cancer patients who received treatments guided by our approach had clinical benefit, including improved response and survival.
Expanding into the real world
Functional precision medicine opens new paths to understanding how cancer drugs can be better matched to patients. Although doctors can read any patient’s DNA today, interpreting the results to understand how a patient will respond to cancer treatment is much more challenging. Combining drug sensitivity testing with DNA analysis can help personalize cancer treatments for each patient.
I, along with colleague Noah E. Berlow, have started to add artificial intelligence to our functional precision medicine program. AI enables us to analyze each patient’s data to better match them with tailored treatments and drug combinations. AI also allows us to understand the complex relationships between DNA mutations within tumors and how different treatments will affect them.
My team and I have started two clinical trials to expand the results of our previous studies on providing treatment recommendations through functional precision medicine. We’re recruiting a larger cohort of adults and children with cancers that have come back or are resistant to treatment.
The more data we have, the easier it will become to understand how to best treat cancer and ultimately help more patients access personalized cancer treatments.
Diana Azzam is a co-founder and owns shares in First Ascent Biomedical. She receives funding from Florida Department of Health and National Institute of Health.
Advertisement

Advertisement
Contact Us
If you would like to place dofollow backlinks in our website or paid content reach out to info@qhubonews.com